Table 1 
List of a) scientific presentations and b) programme presenters included in the Corpus JAPAC-ASCVD programme
|
a) Presentation titles
|
b) Programme presenters Prof. Steve Nicholls*Prof. Brian Tomlinson* Prof. Shizuya Yamashita* Prof. Christie Ballantyne Prof. Alberico Catapano Prof. Gaetano de Ferrari Dr. Robert Hegele Prof. Ulrich Laufs Prof. Marc Sabatine Prof. Lale Tokgözoğlu Prof. Anne Tybjaerg-Hansen |
|---|---|
| * JAPAC-ASCVD Programme Scientific Committee member. | |
Impact assessments
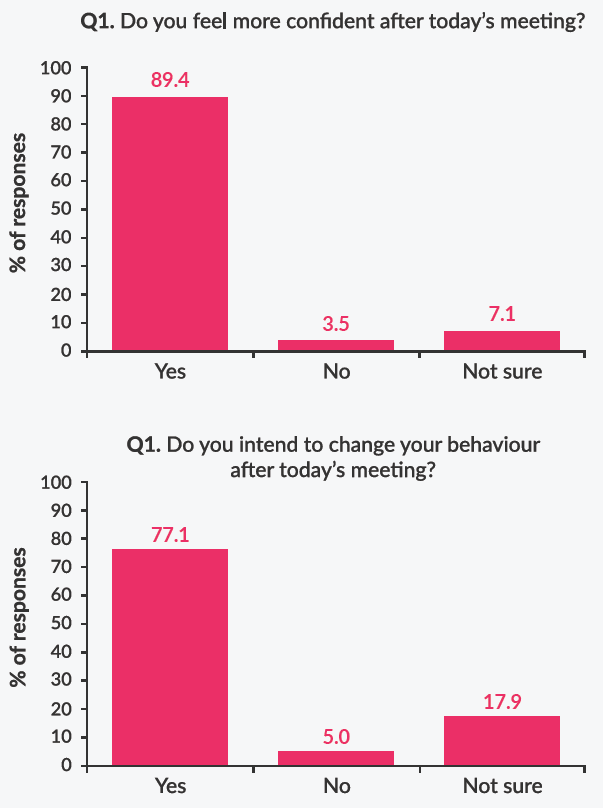
Impact measurements were applied across all JAPAC-ASCVD meetings to assess perceived educational value and behavioural change among HCPs across four key assessment areas:
1) effectiveness of knowledge transfer;
2) intent to change behaviour;
3) perception of educational value;
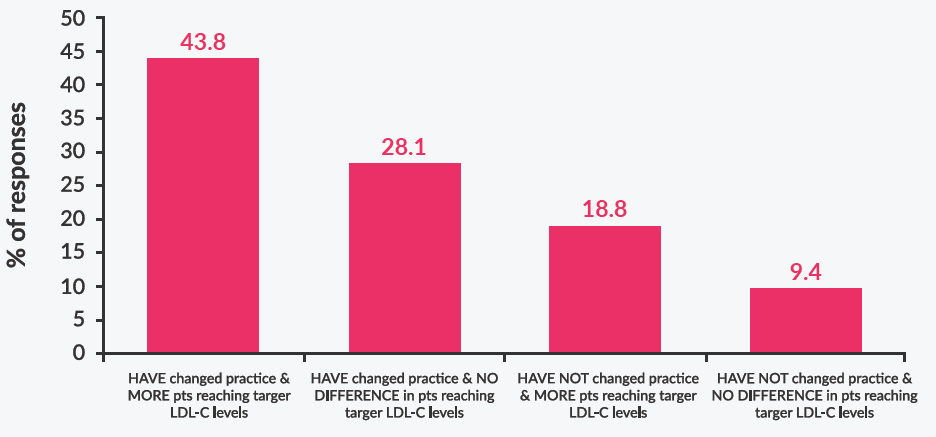
4) self-reported actual change
in behaviour.
Data were collected using 1–2-page pre- and post-meeting questionnaires that were developed by the programme scientific committee in collaboration with the programme organisers, and which were made available to meeting attendees via QR code access on their personal devices.
Pre-meeting questionnaires assessed initial HCP understanding of the intended scientific topics (Table 2). Questions regarding physicians’ current medical practice in terms of treatment choices and treatment to target LDL-C levels in ASCVD patients were also included in most meetings.
To maximise engagement and enable measurement of knowledge transfer, attendees were also asked questions that were specific to the scientific content of each presentation. These presentation-specific questions were formulated to solicit responses that were either factually correct or incorrect, enabling semi-quantitative comparisons before and after
the presentations.
To assess the success of knowledge transfer after each meeting, HCPs were
1) Did you change your clinical practice behaviour as a result of the Corpus JAPAC-ASCVD meeting?
2) Are more of your patients now reaching target LDL-C levels?
Data analysis
Programme attendee responses were collated and underwent semi-quantitative analysis based on a categorical data set. Data are presented as numerical values (from binary count of responses to pre-defined questions) and calculated percentages (relative to total audience per meeting). Percentage changes in questionnaire responses before and after the meeting, and between assessments conducted at the meeting and at 1-month follow-up, are also presented. By nature, this was a retrospective analysis, so no pre-defined statistical analyses were conducted.